|
Dr. Jyoti Patel, MD Functional Medicine Doctor Gut Health & Wellness Expert |
Gut Brain Axis | Imbalances | Symptoms | Causes | Diet | Genetics | Trauma | Stress
Nearly one in five U.S. adults lives with a mental illness.[1] Not to mention, so many of us are not living the happy, joyful lives we all desire and deserve. With so many lives affected by less than ideal mental health, is there anything we can do to improve our emotional well-being?
A common misconception about mental health is that it’s separate from our physical wellness. We have enough research available to know that the mind and body are intimately connected.
In this article, we will look into the connection between digestive health and our emotional wellness. We will also discuss how to know if your mental health is affected by common gut health issues, including some key powerful lifestyle changes you can make to support your digestive health and well-being.
Disclaimer: Keep in mind, that not all mental health issues are related to the gut. There are cases where conventional prescription drugs are still needed for mental illness. Use the information in this article to educate yourself and speak with your doctor to see which options apply to you.
The Gut is Our First Brain
“All Disease Begins in The Gut.”
-Hippocrates, the father of medicine
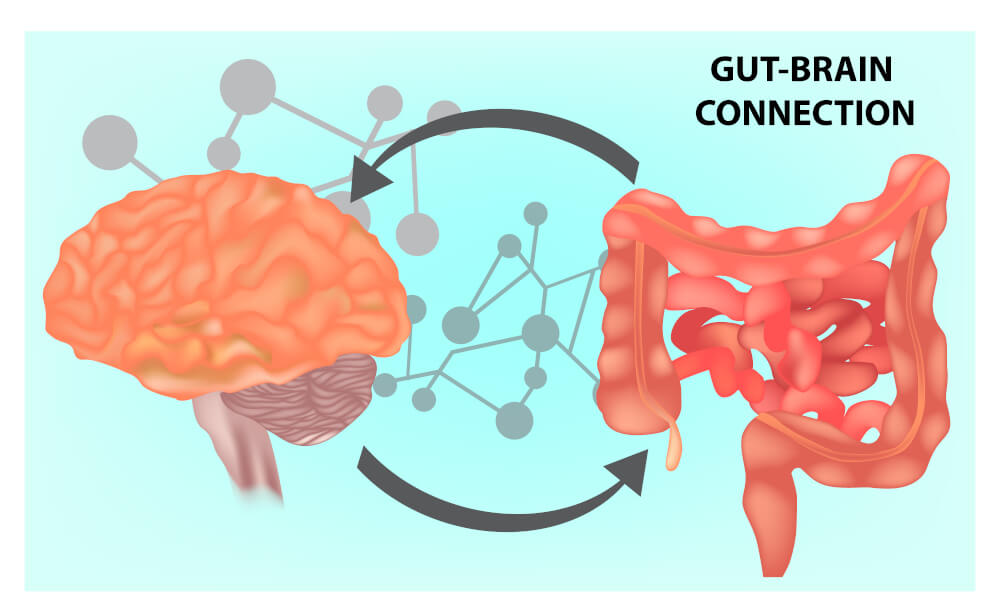
Health starts in the gut. From the days of the ancient Greeks to today’s modern science, we have plenty of evidence that links multiple diseases to compromised gut health. But what about our mental health? Known as the gut-brain axis, there is a bidirectional communication between the central and the enteric (intestinal) nervous system that links the emotional and cognitive centers of the brain with peripheral intestinal function.[2].
Just to give you a few examples of how intimately our brain and gut are connected:
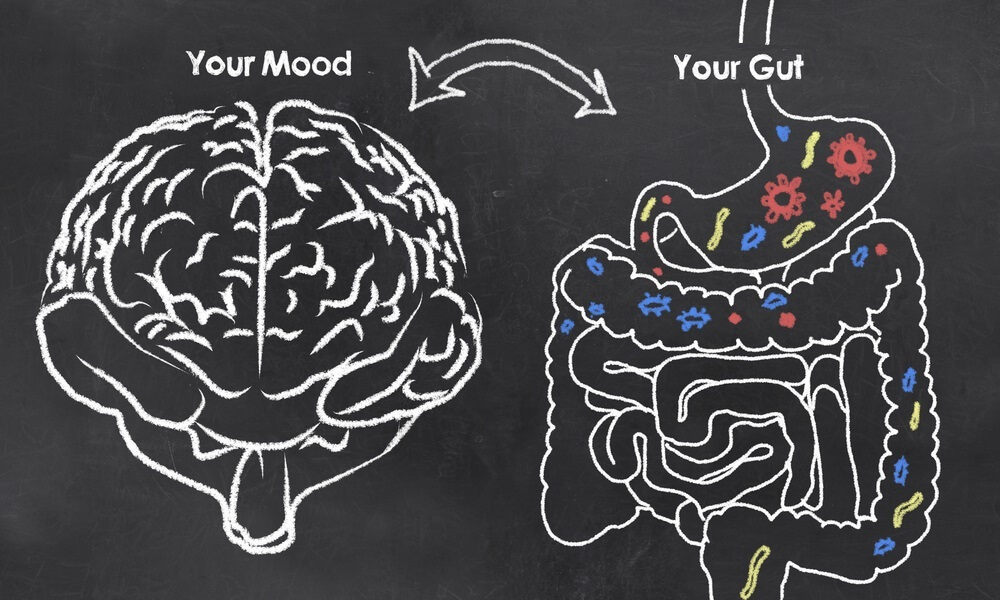
- 90% of serotonin is made in the gut:
Known as the happy hormone that regulates our mood, 90% of serotonin is made in the digestive tract, not the brain! - The gut microbiome makes key mood-boosting neurotransmitters:
Our gut bacteria produce neurotransmitters such as dopamine, norepinephrine, acetylcholine and GABA, which all play a critical role in our mood, motivation, and concentration. Imbalances of these important neurotransmitters are linked to anxiety, depression and other mental health issues. Animal studies of fecal transplants showed that a healthier microbiome post-transplant resulted in improved mood.
Fascinating, isn’t it? You must be wondering at this point how exactly we ended up with a physiology where our brain health is so deeply connected to our gut health. Isn’t the brain supposed to be in control of our mental health?
It is important to understand that no system in the body works in isolation. Our digestive tract is the most primitive and earliest part of our physical development. Often referred to as our “first or early brain”, our gut is connected to every system in the body through the nervous system. Our gastrointestinal system has a hundred million nerve cells, more than the spinal cord or peripheral nervous system. One of the connections in the gut includes direct communication via the vagus nerve to the brain.
Gut Brain Axis Imbalances & Mental Health
Gut-brain axis issues can affect the entire body, so there may be symptoms that at a first glance, do not even seem connected to poor gut or mental health.
It is very important to have all your health concerns evaluated and to avoid treating individual symptoms that may be interconnected, separately. A stubborn skin rash and digestive issues coupled with anxiety or panic attacks, for example, may be caused by an imbalance in the gut brain axis.
So, how do we tell if there is a problem with the gut-brain axis? In functional medicine we review all the symptoms and concerns present, and together with the relevant lab tests, we look for imbalances to identify the root cause. The symptoms may vary from one person to another depending on the unique way their body deals with gut-brain dysfunction. The treatment is then tailored to address these unique factors.
Symptoms of Gut Brain Axis Issues
Below are some of the more common symptoms that may indicate an issue with the gut brain axis. Keep in mind, this is not meant for you to self-diagnose, but just as an example of how the gut-brain axis can affect both our physical and mental health.
Digestive issues
- Acid reflux, indigestion, bloating, constipation or diarrhea, abdominal pain, cramping.
- Undigested food in stool
- Food sensitivities
- Pain after eating certain foods.
How you feel
- Mood swings such as depression, anxiety
- Insomnia
- Fatigue, low energy, sluggishness
- Muscle tension
- Chronic pain.
Other symptoms
- Unintended weight changes, difficulty losing weight or weight gain
- Skin issues
- Hair loss, early graying
- Dry mouth
- Blurred vision
- Asthma
- Difficulty swallowing
- Infertility, menstrual irregularities.
Four Common Causes of Gut Brain Axis Imbalances & Mental Health Issues
1. Modern Diets & Our Mental Health
The foods we eat play a key role in our gut health and emotional wellness. Modern diets are packed with chemicals, toxins, additives, and ultra-processed foods that can disrupt the gut microbiome and affect our mood and cognitive function. As if that’s not enough, these unbalanced diets often lack critical nutrients, vitamins and minerals that are essential for physical and mental health.
Some of the tests I use when starting to evaluate a patient’s nutritional & gut health include:
- Micronutrient deficiencies analysis. Low levels of certain vitamins, minerals, fatty acids, and amino acids that can affect brain function and emotional health.
- Comprehensive stool & microbiome analysis. How healthy is your microbiome? Are there any imbalances that may contribute to mental health? These tests look for evidence of bacterial overgrowth, pathogens, malabsorption, or deficiencies. Certain types of gut dysbiosis such as small intestine bacterial overgrowth (SIBO), for instance, can affect your mental health and brain function.
- Heavy metal toxicity. Heavy metals can come from either the diet or the environment. This is another factor that can have a profound impact on mood, the ability to focus, and on mental health.
2. Genetic Variations

Due to genetic variants, some people can’t effectively process stress hormones such as cortisol and adrenaline. As a result, they end up with a prolonged stress response that affects their mental and overall health.
When the body can’t clear stress hormones fast enough, they linger in the system much longer. As a result, a normal stressful event (physical or emotional) that usually causes a short temporary “fight or flight” response can turn into a heightened stress response.
For example, let’s say you hit the brakes hard to avoid a collision on your drive home from work. It is normal to have an immediate rise in heart rate or blood pressure. But, for those who have an imbalanced stress response, days later they are still feeling the effect of that event, with high levels of stress, anxiety, panic attacks, or depression.
Testing for genetic variations (also known as single nucleotide polymorphisms, or SNPs in short), enables us to better understand the unique situation of each patient and tailor the treatment to bridge these gaps. Certain nutrients such as methylated vitamin B12, vitamin B9 (folic acid) and magnesium, for example, can help the body naturally remove stress hormones and support a healthy stress response for those with genetic variants.
3. Trauma & Mental Health

Childhood trauma can significantly impact mental health and well-being many years down the line. A study conducted by Kaiser Permanente from 1995 to 1997, interviewed over 17,000 adults about their experience with childhood trauma. The study found a strong correlation between a traumatic event in childhood with later in life health and well-being challenges.[3]
This landmark study was one of the first to show a connection between mental and physical health, tying the mind and the body together. These results also show us how important it is to evaluate mental health as a part of our entire physiology. Trauma can get trapped in the body’s tissue, affecting the vagus nerve and the sympathetic “fight or flight” nervous system. Looking into personal family & medical history can help uncover past events and other important factors that are unique to each patient, which may contribute to their current mental health issues.
4: Chronic Stress: When the Panic Button Keeps Getting Pushed

We now have enough evidence to know the devastating effect life stressors have on our health and well-being.
Chronic stress has been linked to hypertension, joint inflammation, cardiovascular disease, poor cognitive function and mental health issues. Therefore, stress is a serious health concern we must take into consideration when evaluating physical and mental health.
To understand how deeply stress can influence our emotional health, here’s a closer look at what happens in our body and brain when we are stressed.
Imagine our ancestors searching for food when all of a sudden, they come upon a large scary bear. In a split of a second, they need to decide; do they fight or flee. The body’s natural fight or flight response is activated.
The fight or flight response is meant to protect us from physical harm. It allows us to make quick, life-saving decisions in a split second. Blood rushes to the muscles to increase power, adrenaline shoots up to increase alertness, the adrenal glands produce the stress hormone cortisol to release sugar for energy into the bloodstream. The only objective is to enhance physical and mental performance in a short-term effort to survive.
Fast forward to modern times, our lives have changed quite a bit since the days of our ancestors. Our basic wiring, however, has not changed. We may not have to deal with large scary predators chasing us, but we live in a culture where we are constantly challenged with stressful events. The body cannot tell the difference between real and perceived stress. Therefore, these events still trigger the same fight-or-flight sympathetic nervous system response.
You can get stuck in a sympathetic tone

And therein lies the problem; the stress response our ancestors experienced was short. Once they felt safe, they stopped and relaxed. The parasympathetic nervous system response was then activated allowing the body and mind to recover, heal and go back to normal function.
Modern life stressors, however, seem to never stop. We wake up thinking about the bear, eat breakfast looking for the bear, keep worrying about the bear all day at work; then when we come home and go to bed trying to relax, we can’t fall asleep because we are still worrying about the bear.
Whether the bear is your boss, the endless chores at home, or financial issues, many people find themselves stuck in this sympathetic tone day in and day out. They may not always be fully aware of it or know how to control it. With our foot on the gas pedal 24/7, we are constantly flooding our system with a tsunami of stress hormones such as cortisol, epinephrine and norepinephrine. This constant flood of hormones is likely the underlying cause of many of the mental health concerns and chronic diseases of our time.
Activating the Parasympathetic Nervous System

Just like our ancestors used their survival instincts to find a safe place where they could calm down, we too need to be mindful about our stress levels and keep them under control.
Activities such as breathing exercises, meditation, progressive body relaxation, movement and exercise, practicing gratitude, all help us feel more loved and connected, and restore balance in our lives.
When we are at that state of mind, our body shuts down the sympathetic tone and increases the parasympathetic “calming” nervous system.
Final Thoughts
Dealing with mental health challenges can be devastating and sometimes discouraging. It is important however, to always have hope! Our body is a self-repairing unit with an amazing ability to heal. When we give it the proper attention and the nutrients it needs, it can get better.
I hope you find this information helpful. Share these tools with your doctor and partner together to create a path to optimal health and wellness.
Read Next
The Gut Brain Axis Diet: a deeper look into some of the key dietary concepts that may help support the gut brain axis, cognitive function and emotional wellness.